Why choose Cook Children’s stem cell transplant program
When your child is facing certain cancers, complex blood disorders, genetic metabolic conditions or immune system diseases, you need an experienced team you can trust. The Cook Children's Bone Marrow and Stem Cell Transplant team has been providing a path of healing to children through life-changing transplants, and peace of mind to their families since 1986.

What you can expect
We perform an average of 50 stem cell transplants a year, making us one of the more experienced programs in the region. Your child and family receive services from the same caring team from start to finish. This close, personal approach means you can focus on what matters most — your child's health — while we take care of the details. We're well-prepared to care for your child, no matter how unique their situation. As a leader in stem cell transplants, you can expect:
Our Stem Cell Transplant Program is accredited by the Foundation for the Accreditation of Cellular Therapy (FACT). It means that we meet the highest quality and safety standards. This commitment guides every aspect of treatment, from pre-transplant testing to post-transplant care. Your child receives trusted care based on standard practices that provide the best results.
We create a transplant plan for your child's unique needs. Their individualized plan includes the pre-transplant preparative regimen (conditioning), donor type considerations and post-transplant care. Experts also consider your child's health at the time of transplant.
We're often among the first places you'll find newly approved options, such as CAR T-cell therapy for hard-to-treat leukemia. We have access to novel agents for maintenance therapy following transplant as well as leading-edge therapy for complications post-transplant if needed. It's part of our commitment to bring the most promising treatments to the children who need them most. Learn more about our Cellular Immunotherapy (CAR T-Cell Therapy) Program.
We partner with your local physician if you're coming to us from outside the Fort Worth area. We share updates with them and plan treatments together so your child receives expert care at home and with us. Great care doesn't stop at our doors. With our guidance, it follows your child wherever they go.
Your stem cell transplant/specialized cellular therapy team
Our team includes the following specialists
- Angela Brentlinger, MSN, RN, CPNP
- Amber Nelson, MSN, RN, CPNP
- Stephanie Tettleton, Stem cell transplant nurse coordinator
- Meg Moffer, Cellular immunotherapy transplant nurse coordinator
- Allyson Kniffin, Stem cell transplant nurse coordinator
- Tracey Easley, Neuroblastoma transplant nurse coordinator
Advancing stem cell transplant care
Our doctors take part in leading research networks, including the Children's Oncology Group, Pediatric Blood and Marrow Transplant Consortium, Clinical Trials Network and the Center for International Blood and Marrow Transplant Research. Our membership in these networks, in addition to other consortiums, gives your child access to clinical trials exploring innovative care options. We also collaborate with pharmaceutical and biotherapy companies to offer clinical trials.
Our research interests include:
- Transplant trials: We're studying new ways to prevent stem cell transplant complications like graft-versus-host disease. We’re also comparing different donor types to improve outcomes.
- Infection prevention: Our team is researching better ways to protect patients from stem cell transplant-related infections.
- Gene editing therapy: We're learning about techniques that aim to correct or overcome the genetic causes of certain blood disorders.
Explore our active stem cell transplant clinical trials.
Hematopoietic stem cells are cells in the body that can turn into any type of blood or immune cell. They can be found in bone marrow (the spongy tissue inside bones), the bloodstream or in the blood from an umbilical cord.
A stem cell transplant, also called bone marrow transplant, involves putting healthy stem cells into your child's body through a vein. The new stem cells can replace cancer cells, such as leukemia and lymphoma. They also help your child's body make healthy blood and immune cells. The transplanted cells can come from your child's own blood (autologous transplant) or a donor (allogeneic transplant), depending on what's best for your child's diagnosis.
Stem Cell Transplant Handbook Page 1-14
If your child needs an allogenic transplant, our top priority is finding the best donor match. We first consider blood relatives, especially siblings. If there isn't a matched sibling, we then consider a parent as well as use the National Marrow Donor Program's large donor and cord blood unit pool. We can access international donor and cord blood registries for additional options.
Before your child's stem cell transplant, we perform a thorough health check and explain what to expect. For families traveling from outside Fort Worth, our team can help you find somewhere to stay.
Treatment starts with medicine (chemotherapy and immuno suppressive therapy) and sometimes radiation to help make room for the new stem cells. This therapy also specifically treats cancer if needed for your diagnosis. On transplant day, we deliver healthy stem cells through a catheter in a central vein. Your child will need to stay in our medical center for on average four to six weeks.
To prevent and manage complications, we give your child special medications, some of which are not widely available. Our pharmacists work with drug companies when necessary to access options supporting the most effective treatments.
Nurses, therapists, child life specialists, dieticians, financial counselors and social workers help make treatment and a lengthy hospital stay easier for your child and family. We coordinate your child's care, answer your questions and connect you with helpful resources.
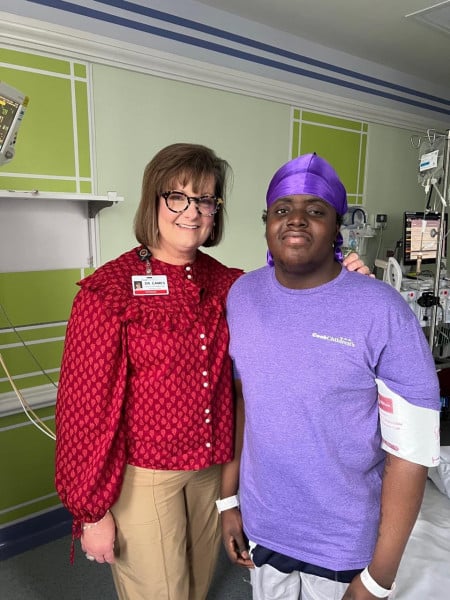
Moments of magic
Hope and healing happen every day at Cook Children’s.