Neurosurgery

When a child with a neurological disorder requires surgery, the experts at Cook Children's Medical Center offer comprehensive care and state-of-the-art technology.
With the help of such state-of-the-art equipment as the revolutionary intraoperative MRI (iMRI), our neurosurgeons are able to determine effectiveness of surgical procedures for cranial and spinal nerve disorders and tailor the treatment to each child's unique needs.
For Dodson Specialty Clinics appointments, please use the new P1 garage to park and check in at the new location of Dodson Central Registration. If you have any questions, just ask us. We're here for you every step! Download map.
Neurosurgeons
Nerves of steel. Hearts of gold. The neurosurgeons at Cook Children's are extraordinary, both for their amazingly skilled hands and for their immense commitment to each and every patient that they treat. They bring a new meaning to the words "medical care." They are relentless in their search for better treatments and cures and in keeping our promise to improve the health of every child in our region through the prevention and treatment of illness, disease and injury.
Conditions treated
Our expanded program includes care across many areas of expertise for pediatric deep brain stimulation, neuro-oncology, stroke and brachial plexus and epilepsy surgery.
- Arachnoid cyst
- Brachial plexus injuries and palsies
- Brain and spinal cord tumors
- Chiari malformation and syrinx
- Craniosynostosis
- Epilepsy
- Hydrocephalus
- Spasticity
- Spina bifida
- Stroke
- Tethered cord
- Traumatic brain and spine injuries
Cook Children's offers some of the most advanced, kid-friendly care in the nation. With leading-edge imaging and diagnostic capabilities, our specialists are able to better treat patients and help them get back to doing what they do best: being kids.
Leading the way in advanced treatments
Brain surgeries are often microscopic, such as revascularization, where doctors take vessels from the external circulatory system of the head and internalize them to make new pathways for blood to flow. Our state-of-the surgical facilities, extremely skilled neurosurgeons, and highly advanced diagnostics all come together to provide your child with world class care during even the most intricate and delicate surgeries.
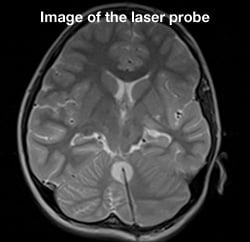
iMRI-guided surgery
Cook Children's is the second pediatric hospital in the U.S. and only the fourth hospital worldwide to build an intraoperative MRI (iMRI) suite using the IMRIS iMRI machine. By combining a specialized surgical suite with this powerful diagnostic tool, surgeons are able to see images of the area of the brain they are operating on in exquisite detail. The surgical team can see tumor size and shape, and distinguish between healthy and unhealthy tissue more easily.
Because the scanner is part of the surgical suite, it moves to the patient inside the operating room so the surgical team can maintain optimal surgical positioning, access and techniques. Being able to look at the area they are operating on during surgery greatly reduces the risk of damaging other areas of the brain and helps to ensure that the entire tumor is successfully removed.
The technology also lets the surgeon take images of the surgical site in the brain before completing the surgery to see if any additional tumor or abnormal tissue removal is needed. If there is, it can be removed during the same procedure, reducing risk of a reoperation.
Using the iMRI allows us to clearly differentiate the tissue targeted for removal whether resecting for tumor or epilepsy.
In addition to tumor resection and epilepsy treatment, the surgical theater has been used for cases of Chiari malformation, conditions requiring deep brain stimulation, hydrocephalus, and other neurological conditions.
Cook Children's has successfully completed hundreds of surgeries using the iMRI. This technology has drastically changed the field of neurosurgery at Cook Children's by making it possible for children to receive the treatment and care they need while staying close to home.
Beyond surgical procedures, the diagnostic portion of the suite has been helpful in ongoing epilepsy patient care and research.
As one of the few pediatric neurosurgical centers with an IMRIS VISIUS iMRI today and one of the largest neurosurgical programs in the Southwest, we continue to find ways to demonstrate our institution's commitment to the care of children with these complex neurological disorders
Laser ablation brain surgery
On May 29, 2013, Cook Children's became the first pediatric hospital in North Texas to perform iMRI-guided laser ablation brain surgery. For the patient, it was a triple win. He was the first to undergo this surgery, and the first at Cook Children's to have this surgery for epilepsy. But the biggest win of all was that just 24 hours after the surgery, the patient was seizure-free and discharged from the hospital. Being the first to perform this surgery wasn't the only benchmark we set that day. We raised the bar on more effective treatment for kids with epilepsy and brain tumors.
Thanks to this minimally invasive surgery, children, teens and young adults no longer have to undergo a craniotomy, or open brain surgery, for certain types of epileptic lesion or brain tumor procedures. And because tumors and lesions are removed by laser without cutting, the level of risk is greatly minimized and the positive benefits of surgery are greatly maximized. Best of all, because the surgery is so minimally invasive, patients can often return home within one to two days of their surgery. Recovery time can also be shortened so that ultimately the kids we treat can get back to business of being kids.
Rare surgery. Extraordinary results.
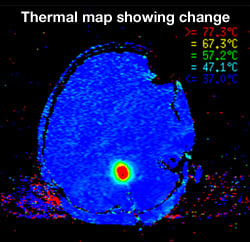
Currently, only 10 pediatric facilities in the U.S. offer this amazing surgery. Also known as stereotactic laser ablation, this iMRI-guided, minimally invasive procedure allows abnormal tissue to be thermally destroyed in real time. The surgery takes place in our iMRI suite, which reduces patient's surgery and anesthesia time and allows for targeted abnormal tissue removal, with little to no risk to surrounding brain tissue. Most patients go home within 24 hours and with only one stitch.
What is laser ablation?
Brain surgery is challenging, and some conditions are more difficult than others. At Cook Children's, we are constantly seeking the most advanced solutions to these obstacles, so we can focus on the most important thing, your child's well-being. Brain tumors and lesions pose a special risk, especially those that are deep in the brain or surrounded by very delicate tissue. For those patients at the highest risk, laser ablation helps the neurosurgeons at Cook Children's precisely target tumors and lesions while reducing, and even eliminating, damage to surrounding brain tissue.
Laser ablation uses targeted light energy to destroy tumors and damaged tissue. Using guided iMRI technology, the doctors can see precisely where the tumor or lesion is in the brain and the laser energy can then be delivered right to the targeted area.
What happens during the laser ablation procedure
- A 3.2mm hole is drilled for cranial access.
- The patient is placed into the iMRI.
- The surgeon guides the laser into position using imaging and then thermally destroys the abnormal tissue.
- The laser applicator is removed and a stitch is placed to close the incision.
Endoscopic neurosurgery
Cook Children's neurosurgeons are constantly searching for ways to improve the care they offer to kids. Over the past decade the use of endoscopy has allowed many children to undergo less invasive procedures, with quicker recovery and similar outcomes to older, larger surgical techniques. Endoscopy involves placing a fiberoptic video camera through small incisions and then using micro-instruments to perform surgery. Some conditions that can potentially be treated endoscopically include synostosis, intraventricular cysts/adhesions, tumors and certain specific types of epilepsy.
The specialists at Cook Children's are constantly assessing children who may be candidates for this remarkable surgery that remains on the cutting edge of neurosurgical care.
Stereotactic EEG
For children, teens and young adults with severe forms of epilepsy, treatment can be very challenging. Often, these patients don't respond to medications or other therapies. For some of them, surgery, such as laser ablation, may provide relief. But before surgery can be performed, a lot has to be learned about the type of seizures they're having and where those seizures are originating in the brain. One of the most effective ways to do this is to implant electrodes into the brain so the doctors can gather the information necessary to determine if surgery is an option. This process is called stereotactic EEG.
In the past, placing electrodes in the brain was invasive and took many hours to complete. But here at Cook Children's, this procedure can be done quickly, very precisely, and it's minimally invasive, making this surgery less stressful for your child. That's all thanks to our robotic arm technology.
Using the very latest in smart technology, the robotic arm is a brilliant tool that takes electrode placement to a whole new level. And while it doesn't actually perform surgery, it does assist the neurosurgeon before and during surgery to ensure that electrodes are placed with never-before-seen accuracy.
Once all the leads are placed, your child is moved to our epilepsy monitoring unit (EMU) and we monitor them by hooking up the leads to our EEG monitoring technology which will gather data on each seizure. Our neurologists process the data and then determine if there's something surgical that can be done to alleviate the seizures.
Before surgery
In any kind of brain surgery, accuracy is always important. To find where epileptic seizures are happening in the brain requires extensive planning and brain mapping to ensure that each electrode is precisely placed. Prior to the surgery, the medical team will take an MRI, and a CT scan. The scans are merged and loaded into the robot's own on-board laptop computer. The computer has a very large screen so the surgical team can plan each trajectory– from where to enter the skull to where to place the electrode lead in the brain.
During surgery
When it's time for surgery, the robot remembers each trajectory so when we go to place our first lead, we tell it which trajectory we want it to go to, and the robot moves into place.
Using its own laser scanner the robot scans areas of the patient's face and then lines it up with the MRI images that have been loaded onto the robot and matches it to the trajectory. It then triangulates itself and tells the doctor exactly where to place the lead.
To place the electrodes, the neurosurgeon drills a small hole about the size of a pencil lead. A special bolt is screwed into that hole. The hair-thin lead then goes through the bolt and the bolt is tightened down to the lead so it stays where it's supposed to.
How seizures are monitored
Once all the leads are placed, your child is moved to our epilepsy monitoring unit (EMU) and we monitor them by hooking up the leads to our EEG monitoring technology which will gather data on each seizure. Our neurologists process the data, pinpoint and then determine if there's something surgical that can be done to alleviate the seizures.
When we combine brain mapping technology with the advanced robotic arm, we are able to more accurately diagnose which children will benefit from brain surgery. Because of the improved data gathered from this testing, we can also identify other potential treatments for children who are not candidates.
Deep brain stimulation
Cook Children's is the first independent pediatric hospital in the United States, and the only children's hospital in Texas, to offer a comprehensive movement disorder program that includes deep brain stimulation (DBS).
Now, we are the first pediatric hospital in the nation to offer DBS on sleeping patients.
Deep brain stimulation, or DBS, is a system that allows the doctor to place tiny electrodes into the brain. The electrodes are connected to an implanted medical device – sometimes referred to as a brain pacemaker – that delivers continuous low-voltage electrical impulses to the targeted part of the brain. These pulses block the abnormal firing of neurons in the targeted area providing relief for patients whose symptoms are not properly controlled by medication.
DBS is used to restore normal function in patients with physiological and movement disorders such as essential tremor and dystonia. The goal of DBS is to reduce muscle tone, improve function and prevent the progression of movement disorders to other areas of the body.
Successful DBS surgery can make considerable improvements to a patient's quality of life, with changes occurring three to six months after activation of the system

DBS doesn't change the way children think or act. But it does stop unwanted neurological impulses that cause involuntary movement.
Imagine putting your arms out and your leg pops up, even though you didn't intend it to. Or trying to make your left leg stay still, but it won't, no matter how much you will it to. Children with dystonia experience all kinds of involuntary movement, and it is often combined with extremely painful muscle contortions, all of which can interfere with even the simple tasks most of us take for granted such as talking, walking, dressing ... even eating. Dystonia and similar movement disorders such as essential tremor can be very, very frustrating for adult patients, and even more so for a child.
Cook Children's offers one of the most recognized pediatric DBS programs available. For many children that we see, DBS surgery can reduce and, in many cases, restore movement, helping our patients to overcome lifelong obstacles.
How is DBS surgery performed?
At Cook Children's, deep brain stimulation patients have both the electrodes and brain pacemaker placed during the same surgery, meaning they only undergo a single session of anesthesia, one hospitalization and one successful operation.
Deep brain stimulation surgery involves two parts: implanting electrodes into the brain and a pacemaker under the skin of the chest. The two devices are connected by the surgeon and electrical impulses are sent from the pacemaker to the brain to correct the abnormal impulses of the movement disorder. At many other hospitals the devices are implanted in two different surgeries and then connected. At Cook Children's, the devices are placed at the same time so the child only has to undergo one surgery.
If your child is undergoing awake DBS surgery, anesthesia is administered during some parts of the surgery. However, during other segments, your child will be awake so that the doctors can test his or her responses to the impulses.
Some children may need to remain asleep during DBS. If that's the case, your child may undergo real-time neurosurgical image guidance and procedure visualization – we call this "asleep" DBS surgery. This is the latest advancement in movement disorder treatments because it means that children who were unable to have 'awake' surgery, may now be candidates for DBS thanks to this new technology.
During the procedure:
- Your child's head rests in the iMRI head coil and fixation frame, while an MRI-visible grid matrix is applied.
- High resolution images are generated by the MRI scanner and sent to the image guidance workstation for the doctor to review and select the neurological target.
- The image guidance software allows the doctor to find an optimal trajectory from the surface of the skull down to the neurological target in the brain, visualizing critical structures to be avoided.
- The grid matrix uses digital intelligence to identify specific coordinates of the entry point for the doctor.
- Once the entry point is created, a smart frame is attached to the patient's head, to help the doctor reaffirm the location of the neurological target and align the trajectory.
- As the surgeon inserts the interventional device through the center lumen of the trajectory frame, real-time images ensure no undesirable events have taken place and the target has been reached.
After awake or asleep surgery, your child will stay at the medical center for a few days then return home. In two weeks, you will return to the medical center where your doctor will turn on the stimulation devices, and adjust them. Over the next few months your child's muscle control will gradually improve and soon they will begin overcome some, if not all, of the difficulties they have experienced for years. It is important to note that DBS patients require regular visits to the medical center for ongoing adjustments to the pacemaker. While this can be time consuming, and create some hardship for patients and families who come from long distances, the benefits for your child can far outweigh the inconveniences.
From diagnosis through rehab in our Movement Disorders clinic, Cook Children's neurosciences team works closely with the patient, the family, and the child's physician to ensure the very best outcome possible.
Since the first implant in 2007, Cook Children's has established itself as one of the elite DBS programs in the nation with a dedicated team including:
- Neurologist with movement disorder experience
- Neurosurgeon with experience in stereotactic localization (operating on a small target)
- Patient liaison
- Physical therapists
- Occupational therapists
- Operating room support
- Skilled nurses
- Anesthesiologists
- Child Life specialists
- iMRI technicians
- Radiologists
- Neuropsychologists
Neurosurgery physician assistants and nurse practitioners:
-
 Hannah Bram
Hannah Bram
PA-C -
 Kari Guffey
Kari Guffey
DNP -
 Nicole Jennings
Nicole Jennings
PA-C -
 Morganna Kuehn
Morganna Kuehn
CPNP -
 Lauren Mouser
Lauren Mouser
PA-C -
 Courtney Porter
Courtney Porter
CPNP
We're here to help.
If your child has been diagnosed, you probably have lots of questions. We can help. If you would like to schedule an appointment, refer a patient or speak to our staff, please call our offices at 682-885-2500.