Exercise Respiratory Center (ExRC)

At Cook Children's Exercise Respiratory Center (ExRC), we diagnose, treat, and research the causes of exercise-induced respiratory symptoms in older children, adolescents, and young adults. Our goal is to remove any barriers created by respiratory causes, so our young athletes can perform at their fullest capacity.
The biggest challenge with correctly diagnosing the cause or causes of EIRS is that testing is usually normal when the patient is not exercising.
To solve this problem, the ExRC is built around maximal exercise testing. The basic idea is to exercise our patients with enough intensity to trigger their symptoms while we simultaneously examine the behavior of the upper airway, lungs, and cardiovascular system. This way, when the symptoms occur, we see precisely where the problem(s) are located, make the correct diagnoses, and start effective treatment with our multidisciplinary team.
The ExRC opened its doors officially at Cook Children's Medical Center - Prosper on October 1, 2023, through an Endowed Chair Award generously given by the Cook Children’s Health Foundation.
What is normal breathing?
The diaphragm is the biggest and strongest muscle for breathing. At rest and during light exercise, the diaphragm is the only breathing muscle needed for respiration. When exercise becomes harder, the body brings in additional muscles of the chest, neck and shoulders, the so-called accessory muscles, to help alongside the diaphragm, increasing the size of each breath further. This occurs in an orderly fashion during increasing levels of exercise: typically, the size of each breath increases first until a maximum is reached, and then the rate of breathing increases.
Download the ExRC referral form Sign up for our newsletter! Contact us
Common exercise-induced symptoms
- Shortness of breath
- Chest tightness
- Cough during or after exercise
- Stridor
- Wheezing
- Dizziness/lightheadedness
Conditions we treat
EILO, (also called Vocal Cord Dysfunction, VCD, or paradoxical vocal fold motion, PVFM), occurs when the voice box narrows inappropriately during physical exertion, usually on inspiration only. This makes it difficult to breathe. There are different ways this can happen: 1) The vocal cords close partially or completely close (glottic EILO), 2) cartilage structures called arytenoids collapse (supraglottic EILO), or 3) both of these occur at the same time (mixed EILO). Symptoms may include rapid onset of breathlessness, noisy breathing, throat tightness, and difficulty breathing in. Typically, symptoms resolve within a few minutes of rest and common asthma inhalers do not provide relief. The gold standard for the diagnosis of EILO is a Continuous Laryngoscopy during Exercise (CLE). Once diagnosis is confirmed, most patients undergo speech therapy to learn both rescue and prevention breathing techniques that keep the vocal cords and upper airway open during intense physical exercise.
DB is an inefficient breathing pattern that causes shortness of breath or other symptoms, including dizziness, chest tightness, sighing, and frequent yawning. DB can manifest in a variety of different ways. Patients with DB might breathe fast and shallow or show a very chaotic pattern of breath sizes and breathing rate. They might rely on their accessory muscles too much (predominant chest and shoulder breathing) and not use their diaphragm efficiently. The way they use their diaphragm and accessory muscles to breathe might be out of sync. Patients might show some or all of these dysfunctional breathing patterns. DB is diagnosed based on symptoms, visualization of breathing patterns by a trained professional, and CPET analysis. Once diagnosed, specialized physical therapy treatments retrain the patient to utilize optimal breathing patterns that involve the diaphragm in every breath.
EIA and EIB combined are the most common causes of exercise-induced respiratory symptoms. EIA is the triggering or worsening of existing asthma by exercise. EIB is common in patients with asthma, but can also occur in otherwise healthy people, including children and adolescents. Both occur when the small airways in the chest narrow during and after exercise, leading to symptoms that may include wheezing, difficulty breathing, chest tightness, and cough. These symptoms are typically worse after exercise is over rather than during exercise. Diagnosis of EIA and EIB includes performing lung function testing before and after exercise or before and after certain stimuli or medication. Once the diagnosis is confirmed, EIA/EIB can be successfully treated or prevented with asthma medication. When exercise-induced respiratory symptoms do not respond to asthma medication, other diagnoses like EILO and DB should be considered. Learn more.
Tests we offer
CLE is the gold standard for diagnosing EILO. A small flexible camera is inserted through the nose to the back of the throat so that the voice box can be seen. Once the camera is secured in place, the patient runs on a treadmill in order to elicit their symptoms so that we can watch how the voice box behaves in real time. We combine the CLE with a cardiopulmonary exercise test (CPET; see What is CPET) during which patients run at increasing speed for approximately 8-12 minutes until they fatigue. We share the video of the voice box with the patient and their family and discuss whether EILO is the cause of their symptoms.
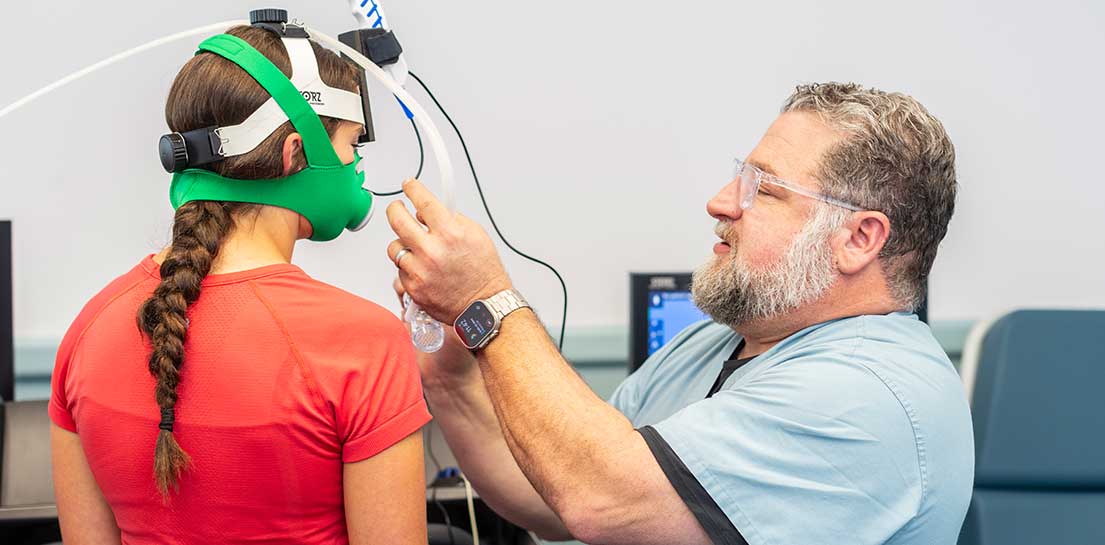
CPET is the gold standard for assessing the health, function, and fitness of an individual’s heart, blood circulation, and lungs (cardiorespiratory fitness and function). To perform a CPET, a patient runs on a treadmill or rides a stationary bicycle while breathing through a mask. This allows us to analyze the amount of air patients breathe, the amount of oxygen they use, and the amount of carbon dioxide they produce when their body creates the energy used to exercise. Additionally, we monitor patients’ blood pressure, oxygen saturation, and heart rhythm. The patients start running at a slow speed. The treadmill speed then increases every 2-3 minutes until the patient has reached their maximal capacity; the entire test usually lasts 8-12 minutes. The information gathered during the test allows us to diagnose cardiovascular and pulmonary causes of exercise-induced symptoms and to measure patients’ cardiorespiratory fitness.
- Complete lung function testing
- Airway resistance
- Diffusion capacity
- Plethysmography (lung volume measurement)
- Spirometry
- Continuous bronchoscopy during exercise (CBE) - The first-ever CBE was performed on a pediatric patient on August 14, 2024, at the Cook Children's Pulmonary Clinic in Prosper, TX.
- Exhaled nitric oxide (FeNO)
- Forced Oscillometry
Services we offer
- Physical therapy for dysfunctional breathing
- Speech therapy for exercise-induced laryngeal obstruction
We collaborate closely with other medical specialties, including cardiology, otolaryngology, gastroenterology, psychology, neurology and sports medicine.
Patient stories
Breathing easier with continuous laryngoscopy during exercise (CLE)
Groundbreaking technique offers breathing relief to young athletes
A breath of fresh air: Teen athlete's breathing condition finally treated
Professional educational resources

Meet our ExRC team
- John Robertson, M.D. - Pediatric pulmonologist
- Andreas Kreutzer, Ph.D. - Exercise physiologist and research scientist
- Ann Nguyen, SLP - Speech-language pathologist
- Amber Brim, DPT - Physical therapist
- Rebecca Brovina, RN - Research nurse coordinator
- Shalyni Ware, RT - Respiratory therapist
- Jennifer Moreles, RT - Respiratory therapist
We're here to help
If your child has respiratory symptoms during exercise, you probably have lots of questions. We can help. If you would like to schedule an appointment, refer a patient or speak to our staff, please call our offices at 682-303-4200 or send a referral fax to 682-303-0719.
Download the ExRC referral form Sign up for our newsletter! Contact us
