Tracheomalacia in children: What parents should know
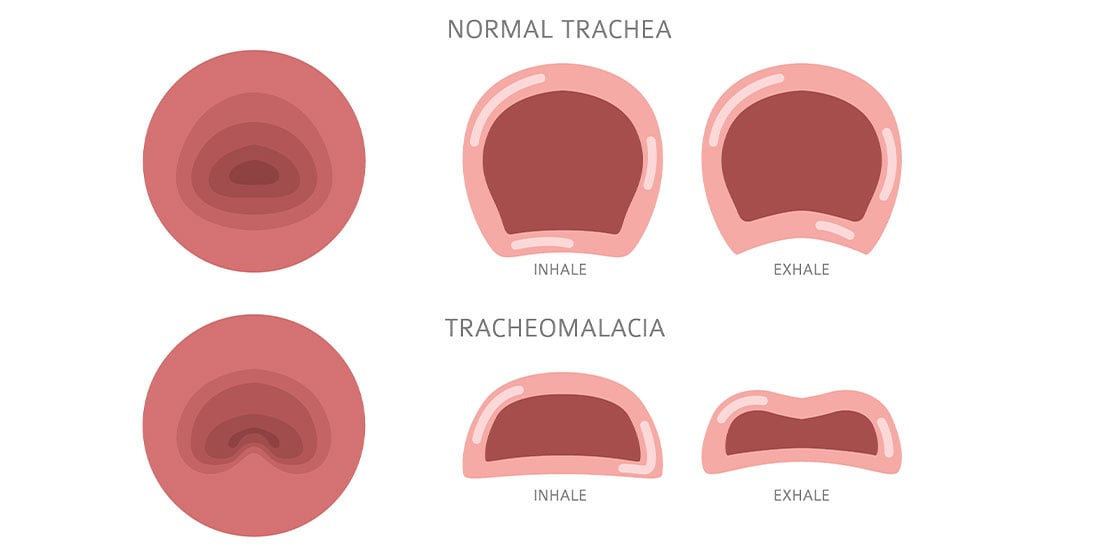
Tracheomalacia is a condition where part of the child's airway is floppy and weak. This can cause the airway to narrow or collapse when they exhale, leading to breathing difficulties, coughing or respiratory infections.
Tracheomalacia may be congenital (present at birth) or acquired (develops later from surgery, infection or other conditions). It can be linked to other conditions such as:
- Esophageal atresia or tracheoesophageal fistula (TEF)
- Vascular rings (blood vessels pressing on the airway)
- An enlarged thymus or other chest mass
- Past infections or tracheostomy tubes
In children with tracheomalacia, the cartilage rings that normally hold the airway open may be soft or abnormally shaped. As a result, the airway can collapse when the child exhales or coughs. When the main/central airway (trachea) collapses, that's called tracheomalacia. When the airway branches (bronchi) collapse, that's called bronchomalacia.
Common symptoms
- Children with tracheomalacia may show various signs. Look for signs like:
- Noisy or high-pitched breathing (stridor)
- Barky or harsh-sounding cough
- Shortness of breath during activity
- Frequent chest infections or pneumonia
- Prolonged recovery from colds or respiratory illnesses
Signs that may be more serious could include:
- Choking while feeding
- Need for oxygen
- Blue spells (lips or face turning blue)
- Pauses in breathing, especially during crying
How's it diagnosed?
Once tracheomalacia is suspected, making an accurate diagnosis is key. Specialists use:
- Dynamic bronchoscopy – A small camera views the airway during breathing, coughing and airway expansion. It is the gold standard for diagnosing tracheomalacia.
- Dynamic airway CT scan – A detailed X-ray-based image of the airway, lungs, and the structures that may impact breathing.
These tests help determine the severity and the best treatment options.
Treatment options
A common misconception is that children outgrow tracheomalacia. This may not be true as the condition may remain the same or worsen in many children. Regular follow-ups and appropriate treatment are key to avoiding lung injury over time. Treatment of tracheomalacia is tailored according to severity.
Mild cases
- Monitoring and regular checkups
- Breathing treatments
- Antibiotics
- Breathing support (e.g., oxygen)
Moderate and severe cases
If symptoms are serious or not improving with medical therapy, surgery may be needed. Surgical options include:
- Posterior tracheopexy – Reinforces the back of the trachea to keep it open
- Anterior tracheopexy – Relieves pressure on the front part of the trachea
- Aortopexy – Moves the aorta to relieve pressure on the airway
- Bronchopexy – Supports the lower airways
- Tracheoplasty – Modifies the airway structure to optimize its patency.
Many surgeries are done as combined procedures for the best outcome.
When to see a specialist
Talk to your doctor if your child has:
- Noisy or difficult breathing
- Frequent and or prolonged respiratory infections
- Respiratory issues not resolving following treatment for asthma or croup
- Trouble feeding or episodes of turning blue
Tracheomalacia may not improve on its own. Expert care can make a life-changing difference.
Professional educational resources
Medical and Surgical Management of Tracheomalacia - With Dr. Pancham and Dr. Mokdad
Expert care is available
At Cook Children's, specialized and dedicated teams provide advanced diagnostics and customized treatment for children with tracheomalacia. Your child deserves the chance to breathe freely. We're here to help. If you would like to schedule an appointment, refer a patient or speak to our staff, please call our offices at 682-303-3350.